International Training Program in Interventional Pulmonology
— Advance Your Expertise in Pulmonary Medicine —
Overview
The Interventional Pulmonary (IP) Medicine is an emerging subspecialty of Pulmonary Medicine that focuses on advanced diagnostic and therapeutic procedures for a wide range of pulmonary and thoracic diseases. This rapidly growing field requires highly specialized knowledge and skills beyond those typically possessed by general pulmonologists.
Recent advances in the field include:
- Endobronchial ultrasound–transbronchial needle aspiration (EBUS-TBNA) for the diagnosis and staging of lung cancer.
- Radial probe endobronchial ultrasound–guided biopsy for the diagnosis of lung nodules.
- Rigid bronchoscopy for various indications.
- Percutaneous dilational tracheostomy (PDT) performed in the intensive care unit.
- Laser therapy and cryotherapy for central airway obstruction, as well as bronchoscopic treatments for asthma and COPD.
- Medical thoracoscopy and indwelling pleural catheter placement for the diagnosis and treatment of pleural diseases.
In response to these advances, the Division of Pulmonary and Critical Care offers specialized training programs at the state-of-the-art Santiwan Respiratory Center, King Chulalongkorn Memorial Hospital.
Learning Objectives
The training focuses on leveraging core competencies crucial for a medical expert who can also function effectively as a communicator, collaborator, manager, health advocate, and scholar. The core competencies include:
- Patient care
- Medical knowledge and skills
- Systems-based practice
- Professionalism
- Practice-based learning and improvement
- Communication & interpersonal skills
What to Learn
A. Patient Care
Trainees must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Trainees will:
- Demonstrate procedural skills in understanding the indications, benefits, contraindications, complications, and general techniques of Interventional Pulmonary Medicine.
- Define the appropriateness, identify the pros and cons of airway stents and Silastic stents, and identify the indications when airway stenting is appropriate.
- Evaluate and discuss procedure options with patients and IP attending in the outpatient setting.
- Perform conscious sedation properly, intubate the airway without difficulty, inspect all airways without interfering with or disrupting the tracheal epithelium, and correctly identify all segmental and subsegmental airways by name and labeling lymph node stations.
- Identify chest wall, pleural, thoracic, and parenchymal lung landmarks and perform thoracentesis under ultrasound guidance.
Trainees will exhibit proficiency in patient care in procedures including the following:
- EBUS – endobronchial ultrasound
- Rigid bronchoscopy
- Therapeutic airway procedures – cryotherapy, APC, laser cauterization, stents and balloon dilation
- Bronchial thermoplasty
- Pleural procedures– medical pleuroscopy, chest tubes, and tunneled pleural catheter placement
- Percutaneous tracheotomy
B. Medical Knowledge
Trainees must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. Trainees will:
- Define the appropriateness and identify the pros and cons among various airway procedures
- Demonstrate advanced knowledge of the anatomy of the thorax as it pertains to various procedures and cite the indications/contraindications, complications, and technique forms of the following procedures:
- EBUS – endoscopic bronchial ultrasound
- Rigid bronchoscopy
- Therapeutic airway procedures – cryotherapy, APC, laser cauterization, stents (metallic and silicone), and balloon dilation
- Bronchial thermoplasty
- Pleural procedures – medical pleuroscopy, chest tubes, and tunneled pleural catheter placement
- Percutaneous tracheotomy
- Demonstrate an investigatory and analytical thinking approach to clinical situations and know and apply the basic and clinically supportive sciences that are appropriate for performing interventional procedures and diagnosing diseases.
C. Practice-Based Learning and Improvement
Trainees must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and life-long learning. Trainees will:
- Demonstrate the ability to use information technology to access the latest medical information and literature regarding the care of their IP patients.
- Analyze data available and weigh the benefits and limitations of the literature to specific patients and incorporate it into treatment plans for IP patients.
- Demonstrate the ability to use the most up-to-date scientific evidence in the care of IP patients by carefully assessing advanced data for the particular strengths or partial strengths of recent thoracic surgery trials.
- Examine own practice for errors and quality of care, conformance with evidence-based standards of care. Know the literature and evidence for how many passes should be performed during a lymph node biopsy, and how to optimize diagnostic yield.
- List the importance of the procedural time-out and implement ways to personally improve planning strategies and preventive measures to reduce errors.
D. Systems-Based Practice
Trainees must demonstrate an awareness of and responsiveness to the larger context and health care system and the ability to call effectively on other resources to provide optimal health care. Trainees are expected to:
- Recognize when to use conscious sedation and when to call upon a larger based team, such as anesthesiology assistance, to help with airway management and display appropriate consult for the use of general anesthesia
- Develop complicated plans and converse on the options for patients, including multidisciplinary approaches, and communicate with ENT, surgical, and IR staff physicians.
- Identify the interdisciplinary resources available, including nurse case management, physical therapy, outpatient rehabilitation, and occupational therapy, to effectively call on system resources to provide care that is of optimal value.
E. Professionalism
IP trainees must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. They are expected to coordinate the team’s activities (with constraints of the above schedule) and provide timely updates, as appropriate and required, to the attending faculty members. They are to fulfill a surrogate leadership role with residents in the absence of the radiology attending. Trainees are expected to:
- Demonstrate respect for patients by providing the highest quality care despite differences in culture, gender, race, or disability.
- Model professional behavior, including punctuality, respectful dress and demeanor, preparation for rounds and conferences, and attendance at conferences.
- Maintain a professional and mutually respectful working relationship with peers, subordinates, and all levels of health care providers within the multidisciplinary thoracic surgery approach discussed above in Systems-Based Practice.
- Demonstrate responsiveness to patient needs and the ability to communicate with IP patients who sometimes rely on additional family members for advocacy.
- Demonstrate compassion and respect for patients, families, and other healthcare providers and maintain security of protected health information.
- Display how to respectfully and appropriately display concern and delegate action to the team for IP patients when instances occur when patient safety is felt to be in danger.
F. Interpersonal and Communication Skills
IP trainees must demonstrate interpersonal and communication skills that result in an effective information exchange with patients, patient families, and professional associates, including nursing staff, respiratory care staff, physical therapy staff, occupational therapy staff, and chaplains. Trainees are expected to:
- Demonstrate diagnostic and therapeutic skills for ethical and effective patient care.
- Concisely and accurately communicate clinical information both in verbal and written form. They will communicate information to patients and family members clearly and compassionately to create and sustain a therapeutic and ethically sound relationship.
- Exhibit expertise in communicating with referring physicians.
- Trainees will consent to patients and discuss the risks and benefits of IP procedures.
- Develop proficiency in communicating with patients and members of the whole team on goals and options of procedures.
Who Should Apply
This course offers pulmonologists the opportunity to enhance their skills in all aspects of diagnostic and therapeutic bronchoscopy, thoracoscopy, and thoracic oncology. Under the close mentorship of leading experts, participants will receive comprehensive training designed to strengthen both clinical and procedural competence.
Eligible applicants must hold a medical degree with board certification in internal medicine and subspecialty certification in pulmonary medicine. Preference will be given to applicants working in academic institutions or public hospitals. A supporting letter from the applicant’s affiliated institution, reflecting the necessity of attending the course, is required. Final candidate selection will be based on the applicant’s curriculum vitae and interview performance. For successful candidates from abroad, submission of a health certificate and valid proof of adequate health insurance coverage is required.
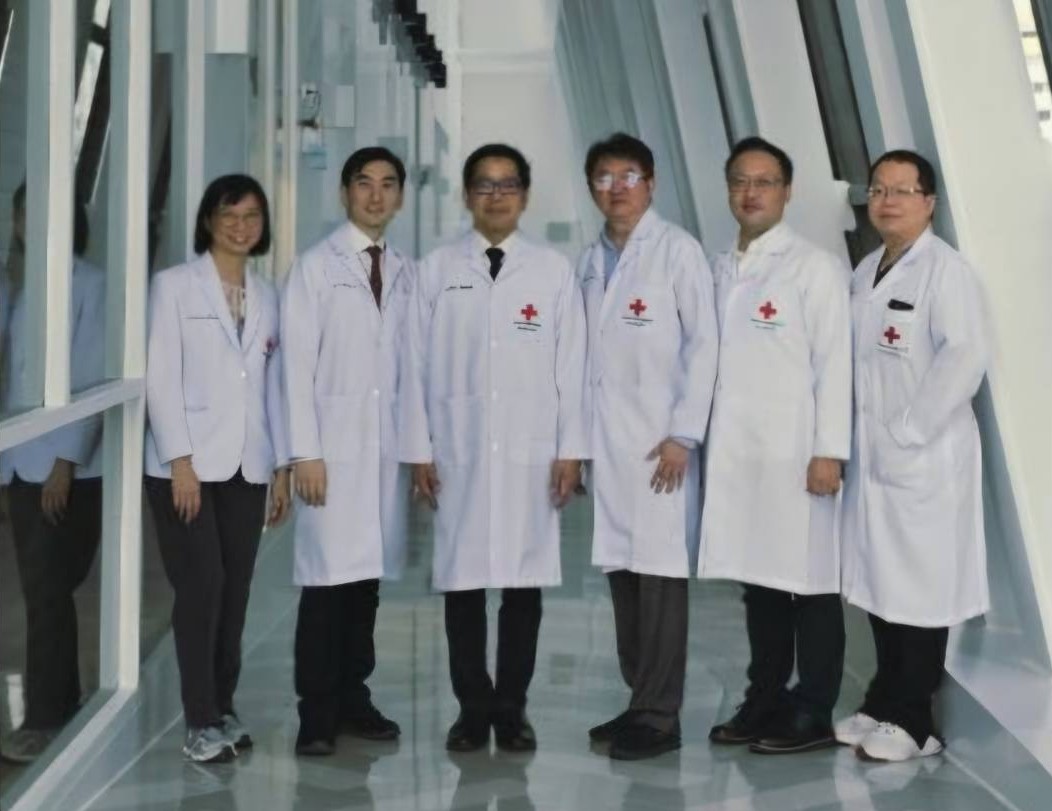
Faculty members
Dr. Thitiwat Sriprasart, MD
Course Director
Division of Pulmonary and Critical Care
Department of Internal Medicine
Faculty of Medicine, Chulalongkorn University
Associated Instructors
- Dr. Virissorn WongSrichanalai, MD
- Dr. Kamon Kawkitinarong, MD
- Dr. Nophol Leelayuwatanakul, MD
- Dr. Vorawut Thanthitaweewat, MD
- Dr. Patnarin Mahattanasakul, MD